As the founder of Atlanta’s renowned Busch Center, Dr. Joseph Busch Jr. brings a 40-year-plus track record in diagnostic radiology and hundreds of international research studies to preventative screening and accurate diagnosis of breast cancer and more recently, prostate cancer. Prior to opening the Busch Center, Dr. Busch, an oncological radiologist, was one of the founders of Diagnostic Radiology Consultants, now known as Prime Imaging in Chattanooga, Tenn. In 2010, he began using multi-parametric MRI to create high resolution and functional images of the prostate to determine the area of restriction of water molecules for targeting cancer. These images are used to perform in-bore MRI-targeted biopsies of the prostate gland. Dr. Busch has read more than 20,000 mpMRI scans and performed more than 1,800 in-bore targeted biopsies of the prostate. He is an instructor at local and international MRI prostate conferences. In this interview with BioTuesdays, Dr. Busch discusses how prostate imaging is changing the paradigm of diagnosis and treatment of prostate cancer and how Profound Medical’s (NASDAQ:PROF; TSX:PRN) recently launched TULSA-PRO device is setting a new standard in customized incision-free ablation of a defined region of the prostate while protecting surrounding tissue in patients with prostate cancer and benign prostatic hyperplasia, (BPH) a non-cancerous enlargement of the prostate gland.
How did you become a proponent of prostate imaging?
About 11 years ago, I attended a conference in Munich, Germany, where Professor Anwar Padhani of the Paul Strickland Cancer Imaging Center in London, England was presenting mpMRI of the prostate. I was impressed with the quality of the MR images and the ability to see the anatomy and function of the prostate that I asked Professor Padhani where I could train to perform and interpret these MR images. He recommended meeting Professor Barentsz at Radboud Medical Center in Nijmegen, Netherland, where I trained in early 2009 on techniques of performing and interpreting mpMRI of the prostate. I returned to Chattanooga and implemented mpMRI imaging of the prostate and in-bore MRI-targeted biopsies. In less than five years, prostate patients were coming to me from all over the U.S. and outside of the U.S. to have their prostates scanned.
What are the disadvantages of current methods of diagnosing prostate cancer?
Studies have shown that 70% to 80% of men with an elevated PSA, or prostate specific antigen, who have a biopsy do not have cancer. However, a PSA test can be appropriate when used with a high quality MRI. Similarly, a digital rectal examine cannot feel 60% of the prostate gland. The third method of diagnosing prostate cancer is a transrectal ultrasound-guided biopsy, which involves randomly sticking 12 needles into the prostate. This method has an error rate of 40% as the needles frequently hit insignificant tumors but miss significant tumors. Some men have had 100-to-150 needles stuck in their prostate and still have missed finding their cancer. On the other hand, a properly executed and interpreted MRI has a 95% negative predictive value.
How do you identify the most effective customized treatment option for best quality-of-life result?
When I started my prostate practice 12 years ago, I thought prostatectomy was the best treatment for prostate cancer. [Prostatectomy is a surgical procedure for the partial or complete removal of the prostate gland.] After interviewing prostatectomy patients for 12 years, I realized the toxicity of prostatectomy, such as urinary incontinence and erectile dysfunction, were much higher than I had thought. It can take six months to recover from prostatectomy and the cancer can return in a couple years. My primary concern is maintaining a patient’s quality of life and that’s one of the reasons I’ve adopted the TULSA-PRO treatment. At the Busch Center, we emphasis personalized care.
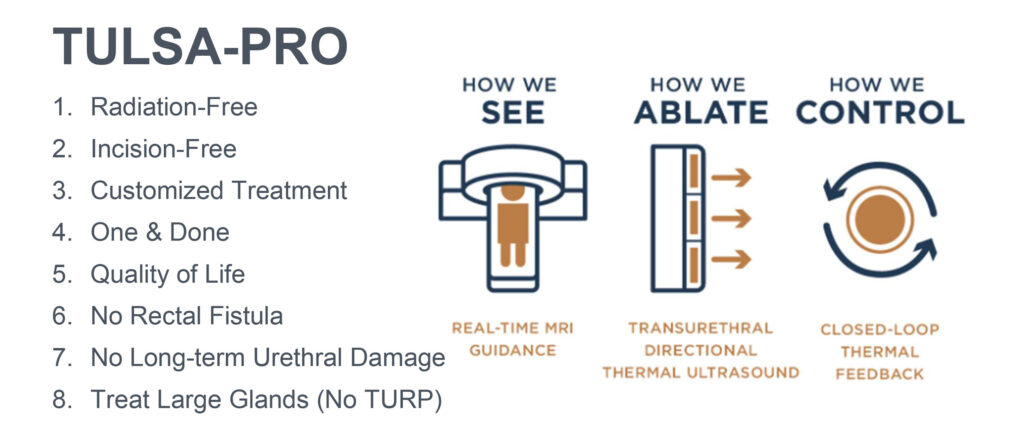
[Editor’s note: Profound Medical’s TULSA-PRO is the only device to merge three modalities – real-time magnetic resonance imaging, direct and controlled thermal ultrasound and close-loop temperature feedback – into a customized, incision-free ablation of prostate tissue while actively protecting the urethra and rectum to help preserve a patient’s natural functional abilities. The TULSA-PRO procedure was approved by the FDA in August 2019 and in Europe in 2016.]
Were you involved in Profound’s TACT pivotal trial in the U.S.?
No, but the pivotal trial results were one reason that I became interested in using TULSA-PRO. I originally took some of my patients to Europe, where TULSA-PRO was already being used, and I was very impressed with the procedure and my patients did very well. They had the procedure in the morning, and we were able to go out for a drink in the evening.
When did you begin using TULSA-PRO?
I have performed 23 TULSA procedures since March 2020. What I really like about TULSA-PRO is that I am looking at multi-planar anatomy and real-time thermal functional imaging. The treatment plan is determined and planned in real time. You can pause the treatment, re-plan and resume during the ablation of the prostate tissue.
What sort of results have you seen with TULSA-PRO?
The 23 TULSA patients have expressed complete comfort and confidence in their treatment procedures, the after care and their initial results, such as sleeping all night without having to get up to urinate. The TACT studies have four years of data showing a 7% recurrence rate with TULSA-PRO, which is substantially lower than other treatments, such as prostatectomy and radiation. The key is early detection of prostate cancer with an MRI, which will improve a patient’s quality of life.
Can you provide more color on quality of life?
There were two qualify-of-life issues in the TACT results that sealed the deal for me: 98% of patients did not experience urinary incontinence and more than 90% of patients had a similar sex life after a TULSA-PRO procedure as they did beforehand. To me, that was the beauty of how TULSA-PRO performed. At the Busch Center, I am offering my patients 25%, 50%, 75% or 100% of gland treatment while targeting the tumor and avoiding damage to healthy tissue. There is no general anesthesia in the single-day procedure, with minimal recovery time. I am the first interventional radiologist in America to adopt TULSA-PRO and our practice is the second in the country to introduce it.
Can you compare TULSA-PRO to another MRI-guided treatment, focal laser ablation?
I was a big proponent of FLA when I first saw it in 2010 and I have probably followed more than 200 patients treated with FLA. It is a good therapy for the appropriate lesion, in the appropriate place. The only problem with FLA is that you can only treat small tumors of eight mm in the treatment zone. TULSA-PRO treats cancerous tissue many times greater than that. What really impressed me with TULSA-PRO was cooling the urethra and rectum during the treatment and avoiding damage in these areas. On the other hand, FLA can cause a rectal fistula, and in radiation and surgery, bladder and rectal injuries can occur. TULSA-PRO stands apart because of low toxicity.
[Editor’s note: Focal laser ablation generates heat to kill a precise spot in the tumor. Under real-time MRI guidance, a special optical fiber is guided into place at the core of the tumor. When activated, the laser emitted at the tip of the fiber destroys the tumor within minutes while special tracking called thermometry confirms the proper temperature. MpMRI scans reveal that the ablation of the tissue is complete, and the laser fiber is removed.]
Do you use TULSA-PRO to treat benign prostatic hyperplasia?
So far, all my BPH patients have had cancer. However, there is a clinical trial being done in Finland that I am watching, using TULSA-PRO to treat BPH. The initial results have been excellent, demonstrating improvement in urinary flow and quality of life. I prefer adoption based on evidence-based medicine, and the Finland evidence is looking very strong. In my opinion, TULSA-PRO is going to be the best BPH treatment you can get.
• • • • •
To connect with Profound Medical or any of the other companies featured on BioTuesdays, send us an email at editor@biotuesdays.com.