Daxor’s (NYSE American:DXR) BVA-100 blood volume measurement device is helping to open a new front in the battle against COVID-19.
“Optimal volume management and knowledge of capillary status is key to survivability, preventing collapse of the circulatory system and allowing time to defeat the infection,” Michael Feldschuh, CEO, says in an interview with BioTuesdays.
Last month, the BVA test was used for the first time to guide blood volume treatment in a patient infected with COVID-19. The company also released a clinical protocol, developed by leading medical experts, for fluid guidance when using the BVA-100 diagnostic test for COVID-19 patients.
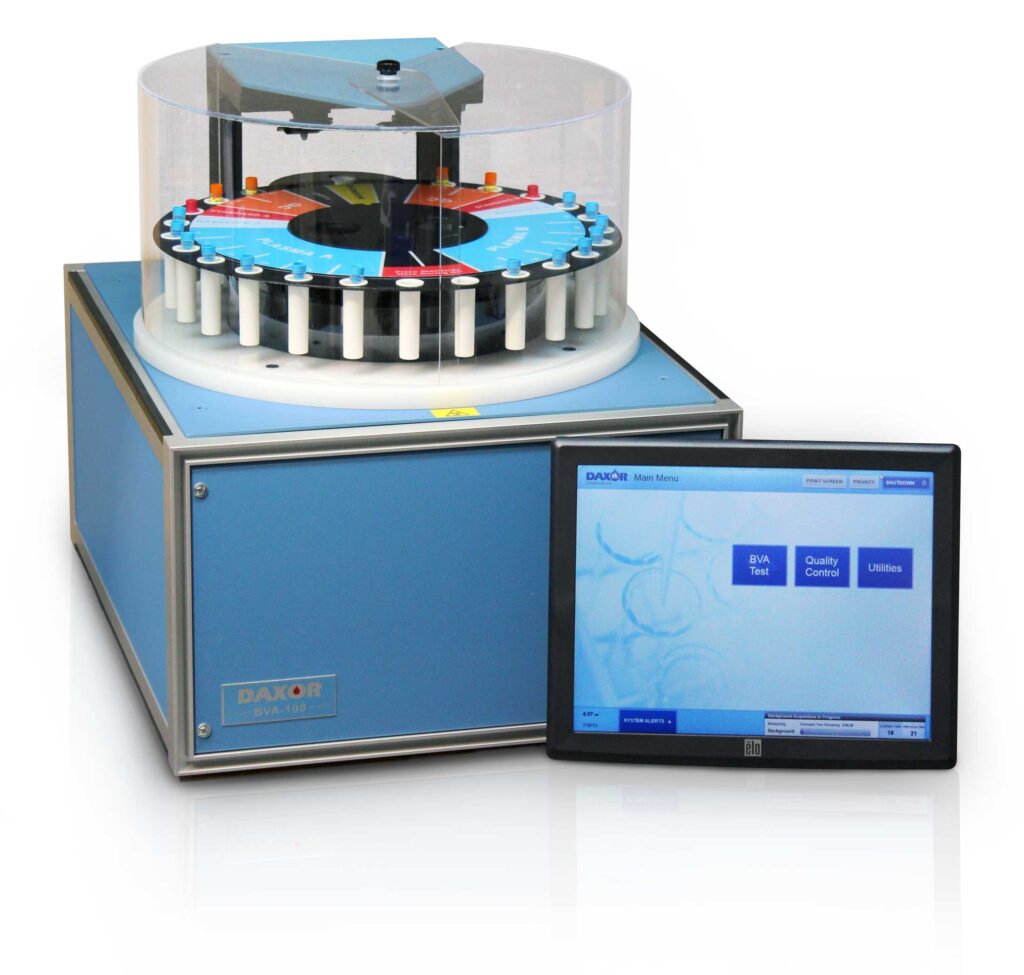
Mr. Feldschuh explains that blood volume analysis is a simple, minimally invasive lab test that involves a few blood draws after a tracer injection that diffuses in 12 minutes. The blood sample is either analyzed with a BVA-100 device in a hospital lab or sent to the company’s lab for analysis.
BVA has been used in over 65 hospitals throughout the U.S. and in more than 45,000 clinical cases and more than 100 research studies, providing results in less than an hour. Blood volume measurement plays an important role in over 18 different areas of medicine, he adds.
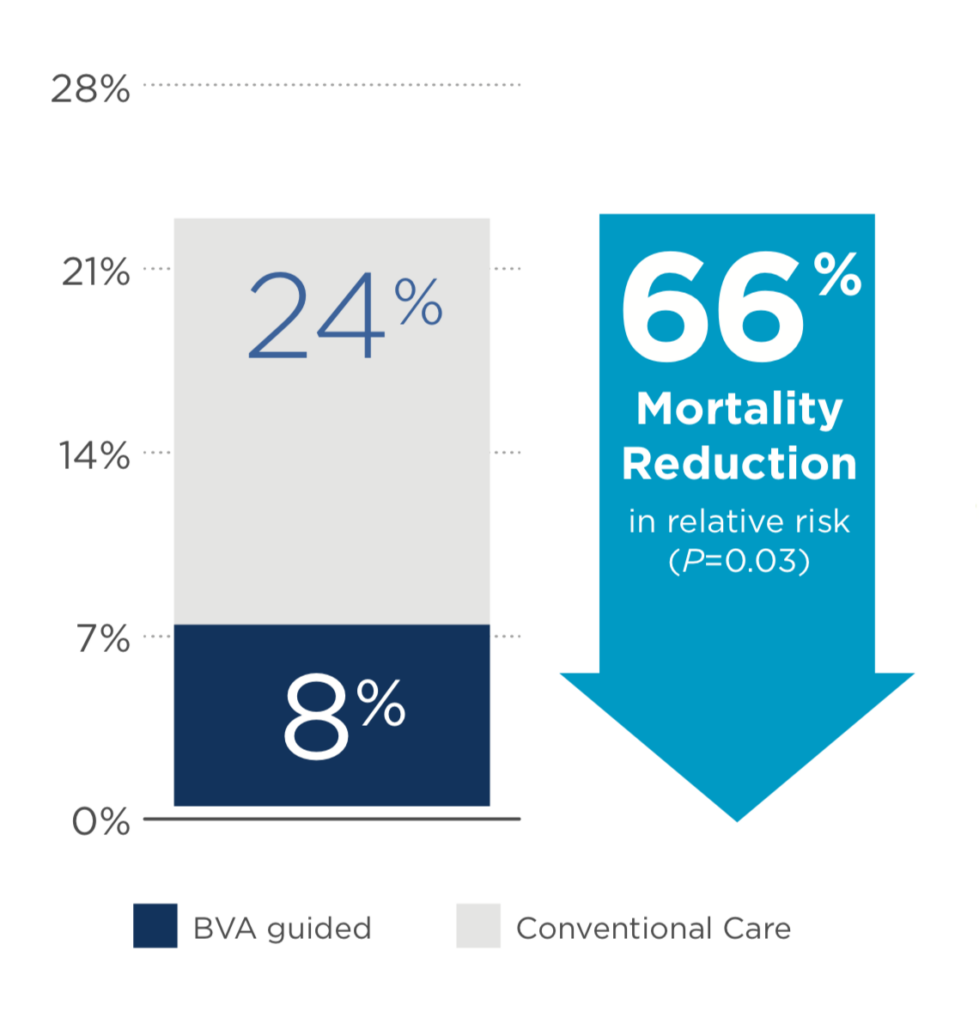
The BVA-100 is the first diagnostic blood test cleared by the FDA to provide safe, accurate and objective quantification of blood volume status and composition including individualized patient norms. It has been shown in a prospective randomized control trial to reduce ICU mortality by as much as 66% and reduce ventilator days in patients suffering predominantly from acute respiratory distress syndrome and septic shock.
Results of the trial were published in the peer-reviewed journal, Shock, in 2011. Among other things, the BVA test reduced usage of ventilators after 45 days by an average of five days and reduced the length of hospital stays by 11 days. “This would play directly into shortages of ventilators and ICU beds in the COVID-19 story,” he suggests.
In addition, Mr. Feldschuh points out that when care teams knew what the correct blood volume was, there was a 44% change in treatment strategy, which is significant. Blood volume analysis improved outcomes and management in the study’s patients, of which 70% and 40% were experiencing severe sepsis and respiratory distress, respectively. “This matters in COVID-19 because patients die from these two things.”
Mr. Feldschuh suggests that Daxor’s test can have a significant impact on patient triage and help precise administration of scarce resources for the healthcare system because of its “unique measure of capillary permeability,” which is common in hemorrhagic diseases and has been shown to have important prognostic value in ICU outcomes.
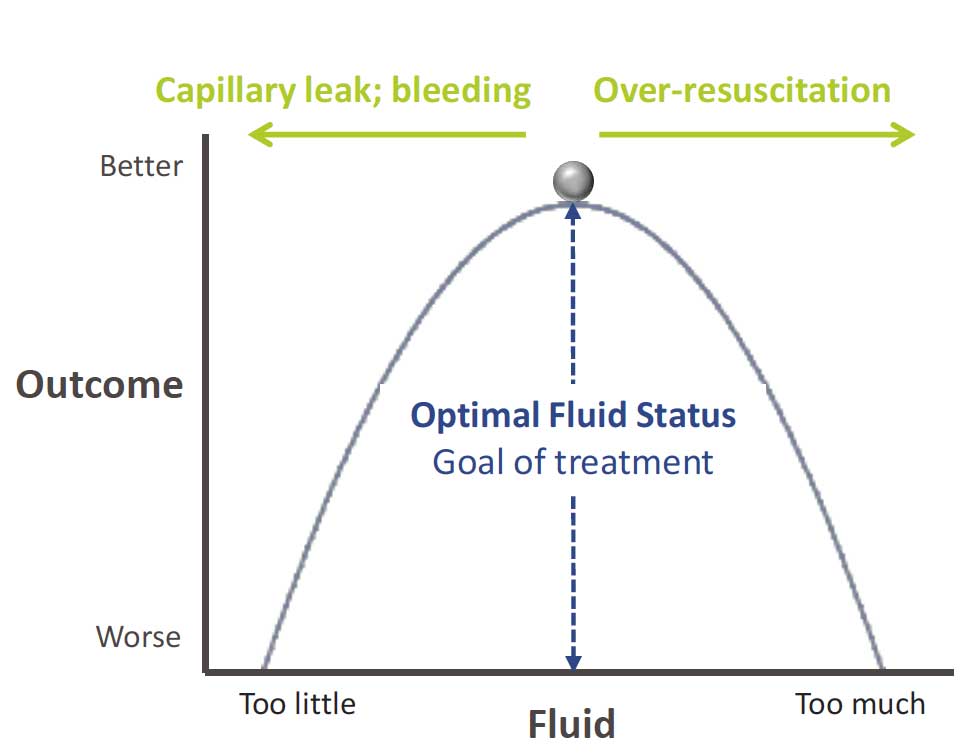
“The BVA test informs care teams and helps guide treatment so they can balance the correct amount of fluids to give patients to maintain effective circulation,” Mr. Feldschuh says. “Patients suffering from acute respiratory distress syndrome are walking a tightrope between receiving too little and too much fluids and their precise red cell volume is unknown.”
Dozens of peer-reviewed studies by the Cleveland Clinic, Mayo Clinic, Department of Veteran Affairs and The Queen’s Medical Center have established the value of Daxor’s diagnostic, confirming that accurate blood volume measurement leads to better informed physicians, better treatment strategies, improved patient outcomes and resource utilization, he adds.
Mr. Feldschuh says three elements are required to keep COVID-19 patients alive: ventilator support to breathe, sufficient cardiac output to circulate hemoglobin-carrying oxygen and adequate circulatory support as measured by blood volume.
“It’s this final point where our test comes in because there’s no point in breathing air into the lungs and pumping fluid if there isn’t sufficient circulation to carry it or red cells to oxygenate. Almost all COVID-19 patients that enter hospital require fluid, many reports also indicate that hypoxia is a problem as well, but the problem is doctors lack a precise and direct measure of volume to determine how much to give them.”
Mr. Feldschuh also points out that coronavirus tends to damage and open capillary walls in patients, causing plasma to leak from the intravascular space into the interstitial space. “If too much plasma leaks out, there will not be enough blood volume to circulate hemoglobin effectively and a patient risks multi-system organ failure, however if too much fluid is given there is also significant risk of mortality.”
According to Mr. Feldschuh, there is currently no other accurate way of directly measuring intravascular volume and red cell deviations of patients and no other test to give the leak rate of capillary walls than the BVA-100 test.
“If we can keep a patient alive long enough for the body’s immune system to mount a credible attack against the virus, a patient would have a better chance of surviving. That’s why patients need ventilators, cardiac monitors and the correct amount and type of fluids,” he contends.
“A virus causing such a highly heterogeneous host response requires a precise, patient-specific fluid approach and we are ready to widely deploy the BVA-100 test at hospitals across the country,” he adds.
• • • • •
To connect with Daxor or any of the other companies featured on BioTuesdays, send us an email at [email protected].