
Perimeter Medical Imaging AI (TSX:PINK; OTC:PYNKF; FSE:4PC) is developing breakthrough ultra-high-resolution, real-time, advanced imaging tools to assist cancer surgeons in achieving clean margins during initial surgery.
“Perimeter’s Optical Coherence Tomography (OCT) technology aims to offer surgeons the most advanced intraoperative margin visualization available, providing clarity on margin status right in the OR versus waiting, sometimes days, for pathology results,” Adrian Mendes, CEO of Perimeter Medical Imaging, says in an interview with BioTuesdays.

Joining Mr. Mendes in the interview is co-founder and Chief Innovation Officer of Perimeter, Andrew Berkeley, who adds, “Intraoperative margin assessment is one of the most pressing issues for cancer surgeons. Perimeter’s mission is to provide them with real-time insights to help make critical decisions, potentially reducing re-excisions, minimizing patient trauma, and saving healthcare costs.”
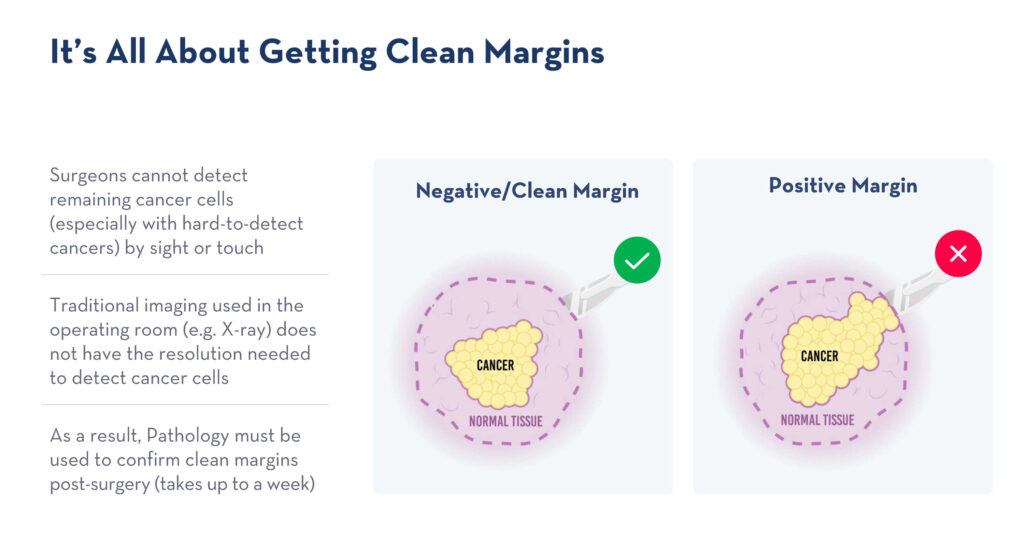
Approximately 200,000 breast lumpectomies are performed in the U.S. annually, with 20% resulting in re-excisions at an average cost of $17,000 per surgery. Together, re-excisions for the top eight cancers, including breast, head and neck, prostate, colorectal, lung, ovarian, kidney, and liver, burden the U.S. healthcare system with $1.2 billion per year.
Mr. Berkeley explains that OCT is a non-invasive optical imaging technique that produces ultra-high resolution of sub-surface tissue structures. OCT is similar to ultrasound, but uses light instead of sound to create cross-sectional, 3D images at ten times the resolution of ultrasound and X-ray, and 100 times that of MRI. A single beam of light rapidly scans the tissue specimen, and reflected light from an up to two-millimeter depth is then transformed into an OCT image.
“It’s a powerful tool for visualizing surgical margins that are often microscopic, including suspicious tissue microstructures and features such as, abnormal ducts,” he adds.
Mr. Berkeley says the portable OCT technology fits conveniently into the surgical suite, allowing it to be efficiently accessed by technical staff or surgeons during surgery. The system includes several components, including optical imaging system hardware, touchscreen software, and an intuitive user interface. To enhance image quality, the light vacuum of the specimen immobilizer helps to keep the surface of the excised tissue securely in place against the imaging glass. The single-use specimen immobilizer or container accommodates samples of up to ten centimeters in diameter and serves to keep them safely preserved for pathology.
Mr. Berkeley contends clinicians have relied on high-resolution OCT imaging for decades to inform their clinical decisions, and it is widely used in clinical settings ranging from ophthalmology and interventional cardiology to dermatology. “Perimeter is the first company to uniquely adapt OCT technology, enabling the imaging of surgical specimens, allowing surgeons to see into the margins in real-time,” he adds.
Perimeter’s commercial-stage S-Series OCT device has received FDA 510(k) clearance under a general tissue indication, which means it has not been evaluated by FDA for use specifically with cancer. Mr. Berkeley points out that the technology has potential for multiple surgical uses and cancer types, including breast, head and neck, prostate, colorectal, lung and bronchus, ovarian, kidney and renal, and liver cancers.
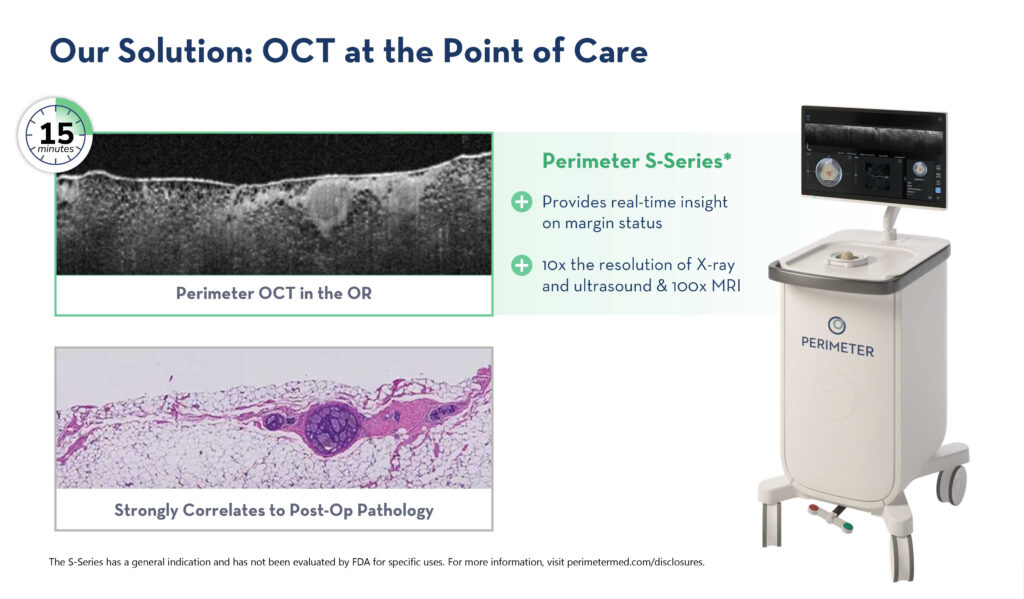
In a recent white paper, the impact of Perimeter’s S-Series OCT device in the OR was highlighted, with study results providing insight into the potential use of it as an adjunctive margin visualization tool to help achieve negative margins during breast-conserving surgery.
“The research demonstrated that in a single-site study of 72 patients, OCT helped achieve a reoperation rate of 5.6%, as compared to the national rate of 19.9%, which is taking it down from about one in every five women needing a second surgery to one in every 18 women,” Mr. Berkeley says. “This is a massive difference, not only for the patient population, but it’s also a real confidence booster for the surgeon going into surgery with this technology.”
Notably, while the national reoperation rate in patients with ductal carcinoma in situ (DCIS) was 30.8%, the recent white paper demonstrated a Perimeter S-Series OCT reoperation rate in patients with DCIS of 13.3%. In patients with invasive ductal carcinoma (IDC), the national rate of reoperation was shown to be 18%, while Perimeter’s S-Series OCT reoperation rate in patients with IDC was 0%.
In addition to OCT imaging, Perimeter’s technology stack includes an AI component currently in clinical trial and an extensive proprietary image library that hosts a plethora of OCT images correlated to pathology, which the company uses to teach readers how to identify key features and in AI training.
“We have been training a dataset of several million proprietary images of both cancerous and healthy tissue captured with our OCT imaging technology,” Mr. Berkeley says. “Our world-class AI team has developed models tailored for real-time applications in healthcare settings and is using our vast image library to train these models to achieve industry-leading results.”
Mr. Berkeley says Perimeter has now layered its first-generation S-Series OCT system with the AI component, ImgAssist, to create the next-generation FDA breakthrough-device-designated investigational-use B-Series OCT.
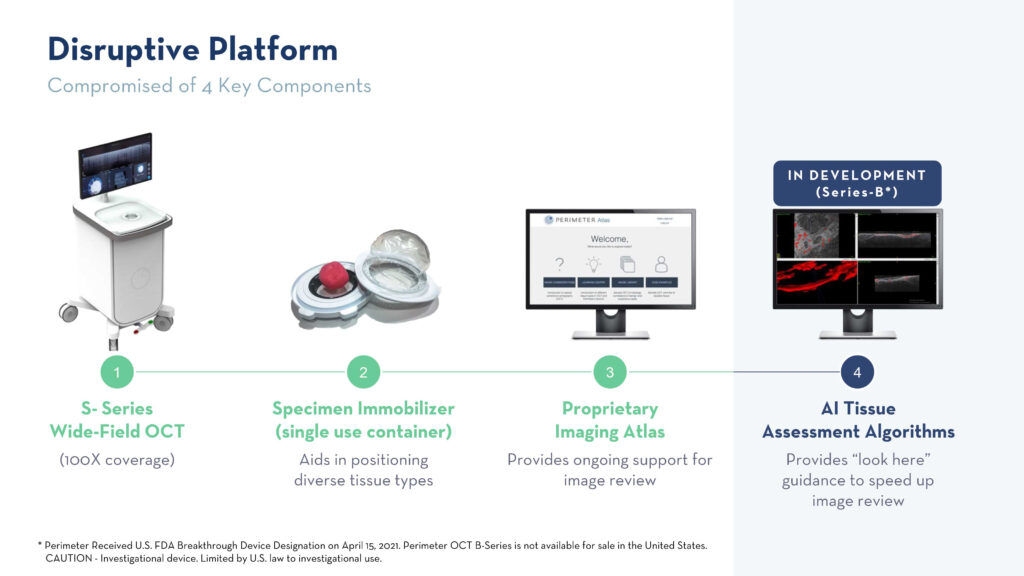
ImgAssist is an AI-driven clinical decision support system designed to enhance productivity and decision-making during cancer surgery.
Mr. Berkeley highlights that earlier this year, Perimeter announced results from a peer-reviewed retrospective study examining the integration of wide-field optical coherence tomography (WF-OCT) with ImgAssist, demonstrating the accurate identification of 96.8% of pathology-positive breast cancer margins. “These results underline the clinical viability of AI-enhanced margin visualization using WF-OCT in breast cancer surgery and its potential to decrease re-operation rates because of residual tumors,” he adds.
An ongoing, multi-center, randomized, two-arm, pivotal clinical study, led by principal investigator Dr. Alastair Thompson at Baylor College of Medicine, is evaluating the use of Perimeter B-Series OCT combined with ImgAssist during breast conservation surgery. Mr. Berkeley informs that the study is being conducted at some of the largest cancer centers in the U.S., including Mayo Clinic, MD Anderson Cancer Center, Moffitt Cancer Center, and Baylor College of Medicine, with completion anticipated by the end of 2024.
“Perimeter’s AI leadership represents a key value driver as we build a product pipeline that aims to improve surgical outcomes and broaden our addressable market through a variety of tissue types beyond breast,” Mr. Mendes says.
“Perimeter’s OCT technology and AI are highly differentiated in that it is well-protected with multiple issued patents and patents pending, with a solid library containing more than two million breast cancer images and trade secrets around how we build our software and algorithms and manufacture our device. So, we have a very nice head start and a bit of a moat around us making it hard for competitors to catch up,” he suggests.
Looking beyond intraoperative care, Mr. Mendes says the company anticipates expansion into the biopsy and pathology markets. “We have the technology to image biopsy samples and apply our AI technology to expedite feedback to the technician or Radiologist. In pathology, we are able to provide a digital image of the entire tumor, so the pathologist is able to identify areas of high cancer probability throughout the region, enabling very targeted sampling,” he says.
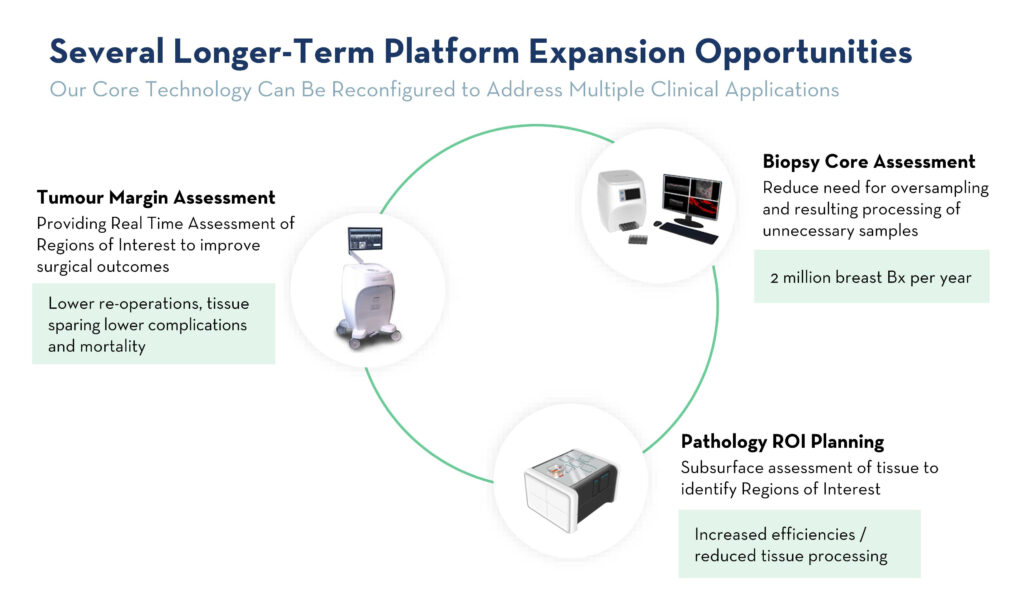
Long-term, Mr. Mendes says the Perimeter team envisions a world where patients no longer experience the emotional and physical trauma of being called back for a second surgery because cancer was left behind.
• • • • •
Editor’s Note:
This information is intended for an investor audience and not for use by healthcare professionals. The information contained herein should not be used to guide clinical practice.
S-Series OCT
The S-Series OCT is indicated for use as an imaging tool in the evaluation of excised human tissue microstructure, by providing two-dimensional, cross-sectional, real-time depth visualization, with image review manipulation software for identifying and annotating regions of interest.
The S-Series OCT has 510(k) clearance under a general indication and has not been evaluated by FDA specifically for use in breast tissue, breast cancer, other types of cancer, margin evaluation, and reducing re-excision rates. The safety and effectiveness of these uses has not been established.
For full information on unapproved/off-label uses, visit: perimetermed.com/disclosures or contact medicalaffairs@perimetermed.com.
B-Series OCT
The Perimeter B-Series OCT System is an adjunctive three-dimensional imaging tool which provides volumetric cross-sectional, real-time depth visualization, coupled with an artificial intelligence computer aided detection algorithm which identifies and marks focal areas suspicious for breast cancer and is used concurrently with physician interpretation of the images. Selene is intended for use in conjunction with other standard methods for evaluation of the margins of an excised lumpectomy specimen during surgical procedures in patients with a biopsy-confirmed diagnosis of breast cancer.
Perimeter B-Series OCT is not available for sale in the United States. CAUTION – Investigational device. Limited by U.S. law to investigational use.
• • • • •
To connect with Perimeter Medical Imaging AI or any other companies featured on BioTuesdays, send us an email at editor@biotuesdays.com.







